By Lambert Strether of Corrente.
Patient readers, I apologize for being late; I got the bright idea of checking the masking policies of the hospitals with which HICPAC members are affiliated late in composition, and although it does nail the post’s thesis, it took longer than I expected.
Still true:
Let’s get the engineering stuff out of the way first, because masking is too important to be left to the medical community. Covid is airborne (a.k.a. aerosol transmission); people infect each other with Covid via “shared air”, which floats like cigarette smoke. Covid is airborne in hospital settings. Masks work to prevent airborne transmission[1].
Infection control guidance for hospitals that deviates from these engineering principles costs patients’ lives. It really is that simple.
As readers know, I have long railed against the hospital infection control community for its tooth-and-nail resistance to the “engineering stuff” summarized above. CDC’s HICPAC (Healthcare Infection Control Practices Advisory Committee) is providing a fine example of massive resistance that, in another context, would have made George Wallace proud[1]. CDC describes HICPAC and its putative mission as follows:
HICPAC is a federal advisory committee appointed to provide advice and guidance to DHHS and CDC regarding the practice of infection control and strategies for surveillance, prevention, and control of healthcare-associated infections, antimicrobial resistance and related events in United States healthcare settings.
Here is HICPAC’s structure, from CDC’s About page:
HICPAC consists of 14 voting members who are not federal employees. These experts are appointed by the Secretary of HHS following an application and nomination process. HICPAC voting members bring expertise including, but not limited to, infectious diseases, infection prevention and control, healthcare epidemiology, nursing, clinical and environmental microbiology, surgery, hospital medicine, internal medicine, epidemiology, health policy, health services research, public health, and related medical fields.
HICPAC also includes six ex officio members who represent federal agencies within HHS, as well as liaison representatives that bring related patient safety expertise from health-related associations, consumer groups, public organizations, and partners. These ex officio members and liaison representatives are included on the HICPAC charter, which is renewed biennially by HHS. Ex officio and liaison representatives are non-voting members of HICPAC.
“Related medical fields” is doing a lot of work there. Since airborne transmission and its prevention are fundamentally engineering problems, some might find it surprising — given that #CovidIsAirborne — that there are no aerosol sciencists or ventilation engineers on the Committee. Then again, if we view HICPAC as the highest expression of the Infection Control hive mind, we might not find it so surprising.
HICPAC is currently reviewing CDC’s guidance on masks and infection control generally, and has already done a lot a lot of damage to patient (and health care worker) safety:
The next meeting is August 22:
There’s nothing now on CDC’s site describing the upcoming HICPAC meeting’s agenda, or when, or how to register, but the Daily Beast (of all sources) has this to say:
HICPAC will meet in August and may vote on proposed updated guidelines for infection control—and it may end up exacerbating concerns rather than assuaging them. An informational slide deck outlining the committee’s proposed updated guidelines, obtained and reviewed by The Daily Beast, makes little mention of aerosol transmission of viruses, and cites what experts say are flawed studies to suggest there is no difference in the protection offered between respirators like N95s and surgical masks.
If accepted, the guidelines could enshrine unsafe practices for health-care workers at a time when the industry is already suffering from critical staffing shortages.
In the section discussing pathogen transmission, there is only a cursory mention of aerosols and airborne transmission, but no real discussion of the types of protection needed for different types of viruses. More shocking, however, is the Evidence Review at the end of the slide deck, in which the studies cited by HICPAC as supporting evidence of its conclusions do not appear to be as robust and persuasive as many public health experts expected.
In a later post, I’ll examine HICPAC’s guidelines more closely. In this post, however, I will examine the Committee itself. Personnel, after all, is policy! Here is the roster of HICPAC members:
(I have highlighted the members whose terms are said to have expired; but since there’s no new roster, I must assume that their terms have been extended somehow.)
I will now go through each committee member, present any relevant publications, and present the current masking policy of each hospital with which they are affiliated. (Unsurprisingly, they are all following CDC’s guidance MR SUBLIMINAL Because CDC is following their guidance, but it’s good to get that on the record. We are, after all, looking at a symposium of infection control titans; it would be surprising indeed if not one institution still implemented universal masking. Or perhaps not so surprising.) I’m going to examine the members a little out of order, because I notice an old friend–
Erica Shenoy, MD, PhD. Shenoy is, of course, one of the authors of this infamous article, reviewed at NC here. I can’t give all the detail, but will quote the essential note [A]:
Here is the key paragraph for Shenoy’s second claim. Since this is yellow wader-level, er, material, I’m going to add some letterered notes, thus “[A]”:
Maintaining masking requirements for [Health Care Personnel (HCP)] during all direct clinical encounters[A] may marginally reduce[B] the risk for transmission from HCP to patient or from patient to HCP. Those potential[C] incremental benefits, however, need to be weighed against increasingly recognized[D] costs. Masking impedes communication, a barrier that is distributed unequally across patient populations, such as those for whom English is not their preferred language and those who are hard-of-hearing and rely on lip reading and other nonverbal cues[E]. The increase in listening effort required when masks are used in clinical encounters is associated with increased cognitive load for patients and clinicians (5)[F]. Masks obscure facial expression; contribute to feelings of isolation; and negatively impact human connection, trust, and perception of empathy (6,[G] 7[H]).
Before going further, I should point out that today masking by staff is common in Asian hospital settings. Therefore, all of Shenoy’s claims are negated for almost half of humanity. If I were so-minded, I’d call out Shenoy for being Eurocentric, or colonialist, or even racist. To the detail–
[A] Shenoy — it seems hardly possible — seems not to recognize that Covid is airborne, spreads like smoke, and is present everywhere, not merely in “direct clinical encounters”; that’s why masking needs to be universal throughout the facility.
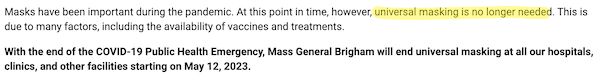
Shenoy is affiliated with Mass General Brigham. Here is their masking policy:
Sharon Wright, MD, MPH. Sharon Wright is a co-author of Shenoy’s vile screed (and I’m not exaggerating). Wright is affiliated with Beth Israel Lahey Health. Here is their masking policy:
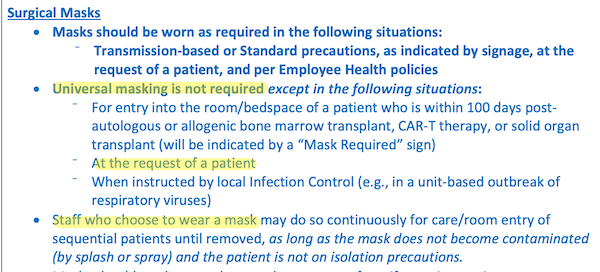
Elaine Dekker, RN. Here are Dekker’s views on masking on April 8, 2020:
We asked Infection Control Director, Elaine Dekker what she does to protect herself. Elaine rides the 9 Muni every day to and from her home in the Tenderloin. Up until last week Elaine did not wear a mask and she continues to not wear gloves. Here are her tips.
Those tips:
One cannot, I suppose, blame even an infection control maven for focusing on fomites and droplet dogma (“6 foot distance,” “close contact”) even in April 2020. I suppose.
Dekker is affiliated with Zuckerberg San Francisco General. Here is their masking policy:
Mohamad Fakih, MD, MPH. Here is a letter from Fakih in Infection Control & Hospital Epidemiology, June 2020:
In times of stress, people also assess their ability to cope with the threat (ie, coping appraisal). Thus, the motivation to engage in protective behavior is heightened with the belief that the recommended protective measures would lead to successful outcomes (ie, response efficacy) and when there is confidence in one’s ability to perform healthy behaviors (ie, self-efficacy; for example, “I am able to constantly perform hand hygiene and mask.”)
Once again, I suppose it’s OK to believe that handwashing prevents Covid transmission in June 2020. I suppose.
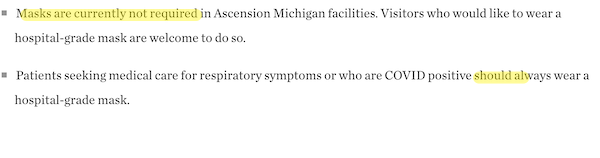
Fakih is affiliated with the Ascension hospital chain at their Grosse Point, MI facility. Here is their masking policy:
Judith Guzman-Cottrill, DO. Here is one article of which she is a co-author, from July 2022:
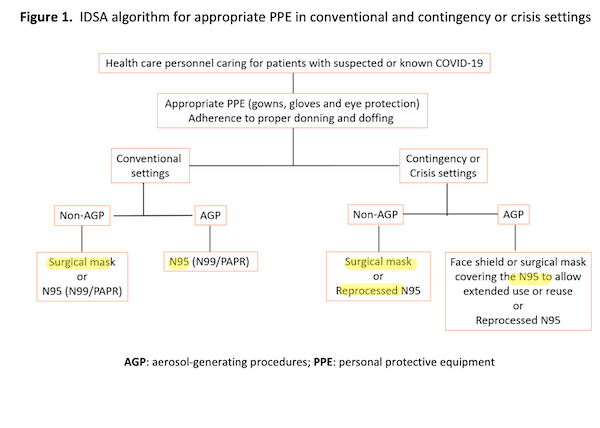
I’m kinda shaking my head at the complexity of this tree structure (and every node has a rent, a concept I shall return to) but at least every leaf (highlighted) recommends a mask of some sort!
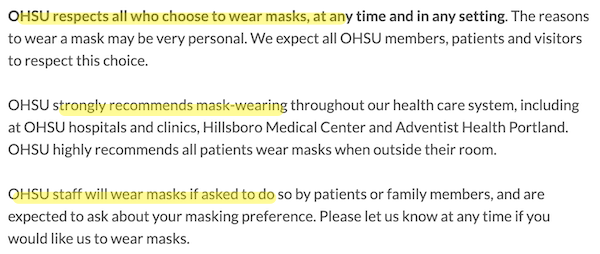
Guzman-Cottrill is affiliated with Doernbecher Children’s Hospital. Here is their masking policy:
JoAnne Reifsnyder, PHD, MBA, MSN. Reifsnyder is affiliated with Genesis, an enormous nursing home chain. I can’t find a Genesis mask policy, or relevant publications from Reifsnyder.
David Jay Weber, MD MPH. Here is a 2023 article for which Weber is a co-author:
One of the lessons learned during the COVID-19 pandemic wasthe important role ventilation plays in the transmission of the virusin healthcare setting. The outbreaks reported among staff, patients,and visitors to the healthcare facility highlighted that attentionneeds to be given to adequate air flow and correct directional flow.The World Health Organization guidance on addressing theinadequacy was a timely help for many during the crisis. There is an urgent call for all healthcare institutions to review the ventilation in all areas, even for daily patient care, because it is fundamental to ensure adequate ventilation to prevent healthcare-associated infections associated with common respiratory viral pathogens such as influenza, respiratory syncytial virus, etc. This review work is best conducted in consultation with the facility engineers and IPC professionals as a team. Inappropriate design of the healthcare facility may often be a root cause for inadequate ventilation. Although there may be specifications for the design in some developed countries, these may be absent in low- and middle-income countries. Nevertheless, it would be expected that a healthcare facility be designed to facilitate safe patient care [lol no].
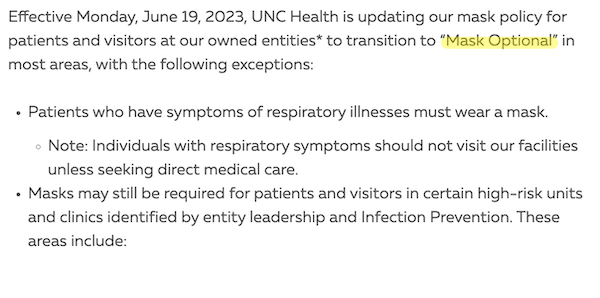
Weber is, at least, sound on ventilation. Weber is affiliated with the University of North Carolina. Here is their masking policy:
Colleen Kraft, MD, MSc. Here Kraft expresses her views on CDC’s 2021 mask guidance:
“So we know the Delta variant can’t get through masks, and so we need to go back to the things that worked, even though we were hoping with increasing uptake in vaccination that people could kind of be able to do their normal activities,” she said.
One question raised during the press conference was whether the U.S. has put too much faith in the vaccinations, especially since states have been unable to increase vaccination rates.
“I think that we needed to put our faith in something,” Kraft said. “I do think that if we had achieved sort of a high vaccination rate, we would have felt that we had been able to stop transmission before the delta variant could have gotten into our borders or come from our borders, whichever way it was transmitted.”
Kraft seems relatively sound on masks (“they work”) but interestingly seems to believe that vaccines halt transmission. Kraft is affiliated with the Children’s Hospital of Los Angeles. Here is their masking policy:
Jennie H. Kwon, DO, MSCI. Here is a 2023 article for which Kwon is a co-author:
Overall, 86% of DHCP [Dental Health Care Personnel] reported having prior training. DHCP increased the use of PPE during COVID-19, specifically N95 respirators and face shields. DHCP reported real-world challenges to applying infection control methods, often resulting in PPE modification and reuse. DHCP reported double masking and sterilization methods to extend N95 respirator use. Additional challenges to PPE included shortages, comfort or discomfort, and compatibility with specialty dental equipment. DHCP found the educational video helpful and relevant to clinical practice. Fewer than half of DHCP reported exposure to a similar video.
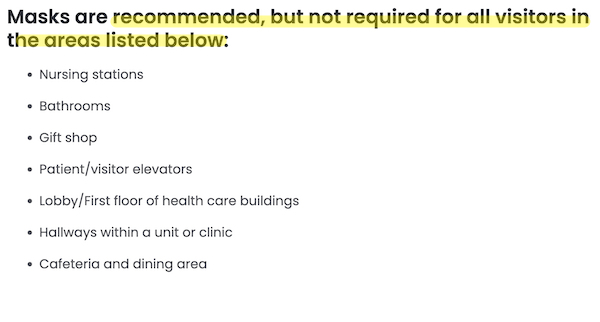
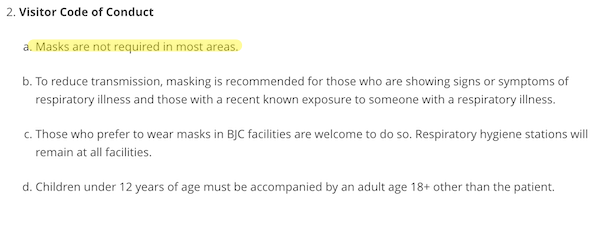
Interestingly, Kwon seems to be the only HICPAC member involved in improving mask uptake and effectivness. Kwon is affiliated with Barnes-Jewish Hospital. Here is their masking policy:
* * *
Some conclusions:
1. None of the hospitals with which the HICPAC members are affiliated have a policy of universal masking.
2. Though some of the HICPAC members look not unfavorably on masking, and on airborne transmission generally, none could be characterized as advocates.
3. Favorability toward universal masking, ideally with N95s, is inversely correlated with institutional clout; Mass General/Brighams vehemently opposed; the University of North Carolina and Barnes-Jewish persuadable.
4. The HICPAC committee members are in the pleasant position of being able to ratify as guidance policies that their institutions have already adopted (i.e., no universal masking, let along universal masking with N95s, going forward). One might, indeed, go so far as to characterize the HICPAC meeting as theatre, were there drama involved in a clearly pre-determined outcome[2].
I would, nevertheless, try to join the August 22 teleconference. There’s nothing wrong with throwing a tomato at a rotten performance!
NOTES
[1] Or maybe the context is the same. Covid infection, after all, disprotionately affects BIPOC.
[2] Going even further, one might characterize HICPAC as thoroughly conflicted.


