With a few notable exceptions—such as during the 1918 influenza pandemic, World War II and the HIV crisis—life expectancy in the U.S. has had gradual upward trajectory over the past century. But that progress has steeply reversed in the past two years as COVID and other tragedies have cut millions of lives short.
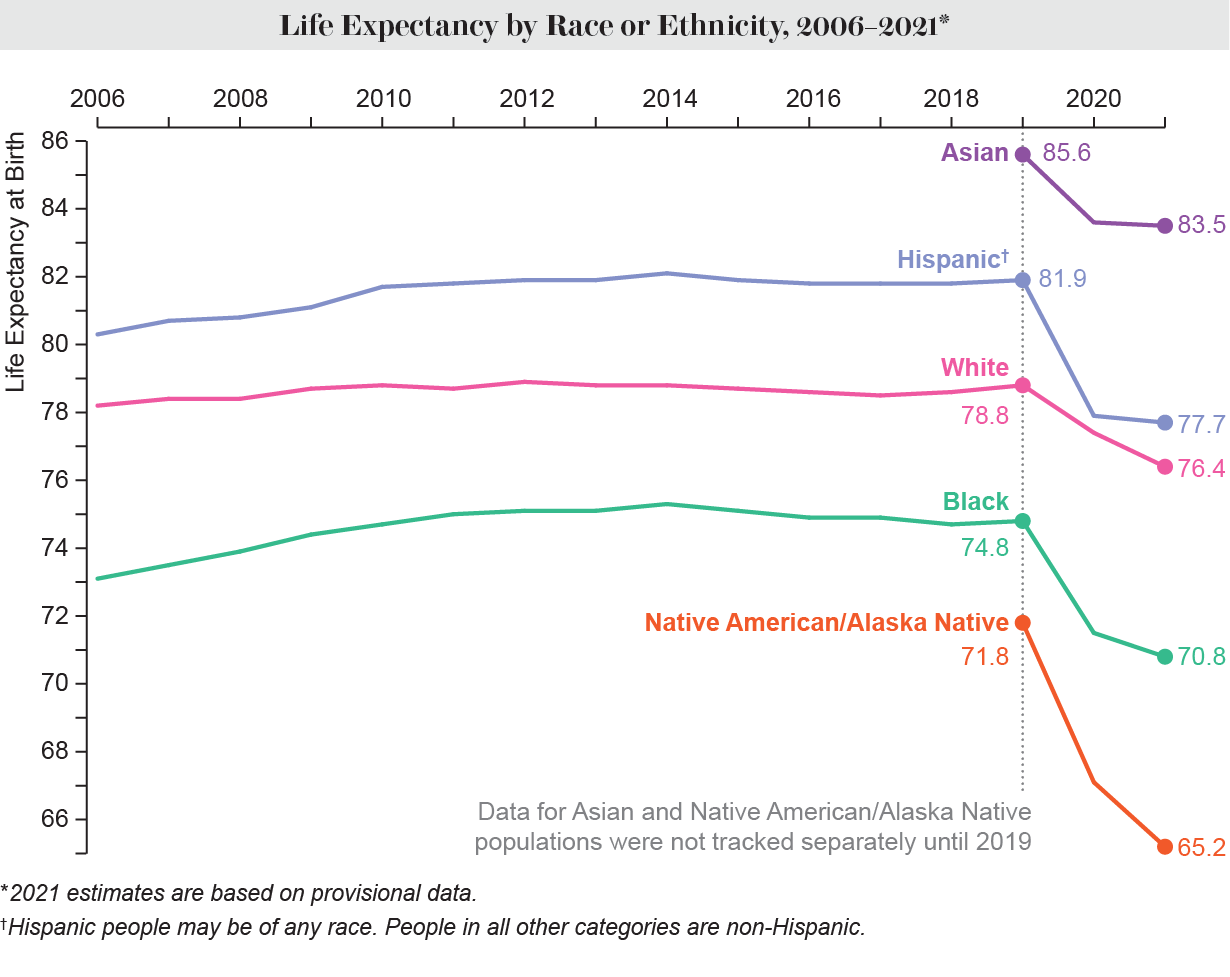
U.S. life expectancy fell by a total of 2.7 years between 2019 and 2021 to 76.1 years—the lowest it has been since 1996, according to provisional data recently released by the Centers for Disease Control and Prevention’s National Center for Health Statistics (NCHS). The drop was 3.1 years for male individuals and 2.3 years for female ones. Non-Hispanic Native American and Alaska Native peoples saw the biggest decline—a staggering 6.6 years. But every racial and ethnic group suffered: life expectancy decreased by 4.2 years in the Hispanic population, by four years in the non-Hispanic Black population, by 2.4 years in the non-Hispanic white population and by 2.1 years in the non-Hispanic Asian population.
Credit: Amanda Montañez; Source: Centers for Disease Control and Prevention
“Basically, all the gains between 1996 and 2019 are as if they never happened,” says Elizabeth Arias, director of the U.S. life table program at the NCHS and co-author of a report on the new data.
COVID deaths drove much of the decline as the country grappled with the world’s worst pandemic in a century. But unintentional injuries—largely driven by drug overdoses—also played a significant role, the data show. Increases in deaths from heart disease, chronic liver disease and suicide also contributed.
“This isn’t supposed to happen,” says Philip Cohen, a professor of sociology at the University of Maryland, who studies demographic trends and inequality. “I think it’s a wake-up call for us … that we can’t put public health on autopilot; that we don’t have this invisible hand of development just raising living standards over time.”
The drop in life expectancy would have been even more stark if it had not been partially offset by declines in influenza and pneumonia deaths, which were likely reduced by pandemic-related precautions such as masking and social distancing.
Arias and her colleagues calculated life expectancy using a technique called a period life table. This involved the researchers imagining a group of 100,000 hypothetical infants and applying the death rates observed for the real population in 2021 for each year of those infants’ lives. The result is not the life expectancy for a cohort of actual babies born in 2021 but rather a snapshot of how life expectancy rates would apply to various age groups at a specific point in time, Arias says.
Credit: Amanda Montañez; Source: Centers for Disease Control and Prevention
The data show that in 2021 the Native American and Alaska Native populations had the lowest life expectancy of any race or ethnicity: 65.2 years. This is equivalent to the life expectancy of the total U.S. population in 1944, Arias and her colleagues wrote. Indigenous peoples, who already had high rates of chronic disease and poor health care access before the pandemic, were disproportionately impacted by COVID.
These outcomes have their roots in colonialist U.S. government policies, says Crystal Lee, an assistant professor at the University of New Mexico’s College of Population Health and CEO of the nonprofit organization United Natives, as well as a health services company called Indigenous Health. “There have just been so many policies that have been harmful to Native Americans throughout all these years,” says Lee, who is Diné and from the Navajo Nation. Native American tribes are officially recognized as sovereign. But they are also still designated as “domestic dependent nations,” meaning they are subject to the U.S. federal government. The government provides funding for education, housing and health care—the latter through the Indian Health Service—but all of these have long been underfunded, according to Lee. “We don’t have the resources or the infrastructure or even adequate medical staffing,” she says.
When the pandemic hit, Lee and her nonprofit organization helped distribute supplies such as masks and cleaning products to the Navajo Nation and the Apache Nations, she says. She also started Indigenous Health to help provide quarantine housing for Native American people exposed to COVID. Many of them had overcrowded housing—or no housing at all—to go back to, and some were struggling with addiction, she says.
 Mourners from the Navajo Nation at a funeral for a person who died of COVID in May 2020. The Navajo Nation and other tribes were hit especially hard by the pandemic, and Native American and Alaska Native peoples have suffered the biggest drop in life expectancy of any group from 2019 to 2021. Credit: Brian van der Brug/Los Angeles Times via Getty Images
Mourners from the Navajo Nation at a funeral for a person who died of COVID in May 2020. The Navajo Nation and other tribes were hit especially hard by the pandemic, and Native American and Alaska Native peoples have suffered the biggest drop in life expectancy of any group from 2019 to 2021. Credit: Brian van der Brug/Los Angeles Times via Getty Images
The second-biggest contributor to the life expectancy decline of the total U.S. population was unintentional injuries, of which a large fraction were opioid and other drug overdoses. Such deaths, as well as those related to alcohol and suicide—sometimes called “deaths of despair”—have spiked in the years leading up to and during the pandemic. Drug overdose deaths reached more than 100,000 annually during the 12 months ending in April 2021. Opioid overdoses were initially concentrated among the white population, but they have now become more common in the Indigenous, Hispanic and Black populations as well.
Cohen says COVID may have exacerbated the opioid crisis because people who lost family members and jobs turned to drugs and may have been less able to access treatment. “One crisis doesn’t wait for another” to finish, he says.
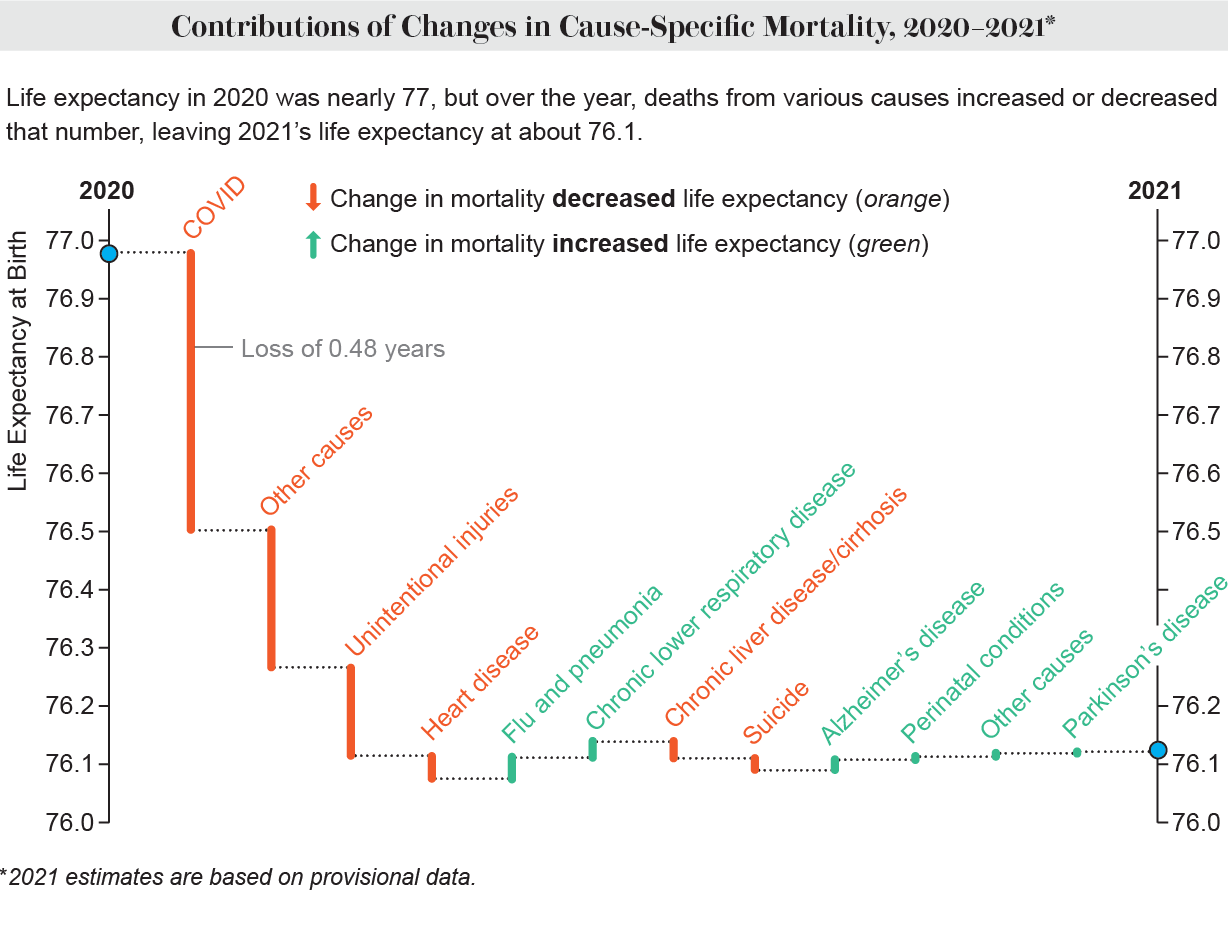
Credit: Amanda Montañez; Source: Centers for Disease Control and Prevention
Native American and Alaska Native individuals, along with Hispanic and Black people, suffered disproportionately high death rates during the pandemic’s first year because many worked in essential jobs with a high COVID exposure risk. But the group with the second-largest drop in life expectancy from 2020 to 2021 was the non-Hispanic white population. Almost half of the total loss of life expectancy of the white population occurred in the pandemic’s second year, Arias says. Lower vaccination rates and more resistance to masking and other precautions among the U.S.’s white population (compared with other races or ethnicities) is one possible explanation. White Americans are more likely to have voted for Donald Trump, and areas that voted for Trump have had higher rates of COVID deaths since the fall of 2020. Additionally, COVID took longer to reach rural parts of the country, which are more likely to have a largely white population.
The gender gap in life expectancy also widened. Historically, women have lived longer than men across every race and ethnicity. The gap between male and female life expectancy had been narrowing in the past decade, however. Women were living 4.8 years longer than men in 2010, but the pandemic erased some of that narrowing, and the gap widened to 5.9 years in 2021. Men are more likely than women to die of COVID, studies have shown. In addition, unintentional injury deaths (largely overdoses)—which have increased—are more common among men.
[embedded content]
Despite being the richest country in the world, the U.S. has one of the lowest life expectancies of any developed country. And it has seen one of the largest declines in life expectancy among such countries during the pandemic, according to World Bank data. Part of this likely stems from a high rate of socioeconomic inequality.
“One of the things that affected me the most—even though I’m used to seeing these numbers … was the fact that there’s such large disparities in life expectancy in the U.S.,” Arias says. The Native American population has a life expectancy comparable to that of some of poorest countries in Africa, she notes. “It’s kind of amazing, when you sit back and think about it, that we have in this country a population that has the same life expectancy as a really poor developing country.”
Addressing these gaps in life expectancy would require the U.S. to overhaul its health care system and make it work for everyone, many experts say. For Native Americans in particular, that means public awareness, allyship and accountability. “We need to hold the U.S. government accountable by honoring the existent treaties,” Lee says. She believes there also needs to be more awareness about Native American people, who she says have become invisible. People need to know, she says, “that we’re still here in the United States, and we’re still existent.”

