Yves here. On the one hand, if you read the business press, you encounter enough discussion of the role of pharmacy benefit managers, or PBMs, to work out that they are very large and profitable and wield enormous influence in the pharmaceutical business…but it’a all a bit fuzzy how they do that.
Kaiser Health News, now rebranded as KFF Health News, has a new article on PBMs, with the news hook that the Senate just held hearings on PBMs before a vote on PBM legislation….with the description of what PBMs do, exactly, and what the legislation entails peculiarly hazy.
Matt Stoller, in his post The Red Wedding for Rural Pharmacies, gave the 50,000 foot description of how PBMs work and how they abuse their monopoly position. A key section:
PBMs handle the drug benefit piece of insurance plans. They maintain a list of drugs for insurance companies, they negotiate drug prices, and they manage reimbursements to pharmacies.
The original idea behind PBMs is they would be able to get enough bargaining power by representing multiple insurance companies that they could negotiate to bring down drug prices. And accumulate bargaining power they did, merging until three PBMs control 80% of the insurance market. They are also vertically integrated with insurance companies and drug store chains. The top three PBMs are owned by CVS, United Health, and Cigna.
Unfortunately, because of an exemption from anti-kickback laws, PBMs don’t use their bargaining power to reduce consumer prices. Instead, they force pharmaceutical firms to compete over who will give the PBM the biggest kickback, which in the industry is known as a rebate. Take insulin. In 2013, Sanofi gave a 2-4% kickback to PBMs to prefer their product to customers. In 2018, that number went up to 56%. In other words, more than half of the price of insulin is going to a middleman who does nothing more than push around paper.
The many bad practices of PBMs are legendary. PBMs often force customers to buy more expensive drugs over their generic counterparts, likely because they get kickbacks when customers do so. This ends up making this obscure group of firms a lot money. The combined revenue of the top three firms, who comprise just a small part of the U.S. health system, is larger than the entire amount France spends on all medical care for its entire population.
It gets worse. PBMs all own mail-order pharmacies, and they are increasingly mandating that patients use those mail-order pharmacies instead of the local pharmacy around the corner. Moreover, PBMs now have so much power they are able to claw back money randomly from pharmacies months after a drug was dispensed, using something called a Direct and Indirect Remuneration fee. (DIR fees are only used for Medicare plans, but that is still 37% of the market.) For independent pharmacies, DIR fees are impossible to plan for, they are opaque, and they end up raising prices for consumers.
More tersely, on Twitter:
17. In return for a higher rebate, a PBM will make your particular form of insulin the preferred product, and so all, say, UnitedHealth Group plan members will be offered that particular brand of insulin, and perhaps not allowed to buy a rival brand, or a cheaper generic one.
— Matt Stoller (@matthewstoller) March 1, 2023
I can’t prove it but I believe the growth of HMOs and then PPOs helped spur the growth of PBMs. The first PBM was established in 1968, soon followed by the HMO Act of 1973. Bills like that don’t appear out of a vacuum; there had to have been a push for that legislation.
The article also bizarrely assumes TINA, as in “There is no alternative” for have to deal with a PBM if you have prescription drug coverage. Their little video starts by intoning (at 0:22) “….if you’re insured, these companies help decide the drugs you get at the pharmacy and what you pay for them.” That is false. I have an indemnity plan and I do not deal with a PBM. I can get any drug my doctor prescribes and choose which pharmacy to use, and prices do vary. Admittedly I am in a minority but this article misleadingly implies there is no way out of PBM hell, when governments could mandate that insurance companies offer non-pharmacy drug plans.
I may be over-relying on the terms of my legacy indemnity plan, which was a pretty typical, not terribly generous employer plan for the late 1980s. It does not restrict me to a network nor does it have a list of preferred drugs or prices. To put it another way, it is not a pharmacy plan. I pay at the pharmacy and then submit for reimbursement. That arrangement forces the patient to lay out cash but it also means the policy-holder is not locked into any pharmacy. The PBM can throw its weight around because it inserts itself between the insurer and patient, and the pharmacy and the insurer.
Could you break the PBMs’ monopolies by having the Feds mandate that insurers offer non-PBM options for all of their Medicare drug plans and Obamacare plans? The problem is I doubt many would take it up unless insurers faced strict penalties for being tardy with claims processing (in theory, it’s five to ten business days after receipt; if they were required to start paying interest if a claim was reimbursed more than a month after receipt, that would get their attention, since the sheer hassle of getting into interest rate computation and payment would help deter foot-dragging).1
By Arthur Allen, a KFF Health News Senior Correspondent, previously worked for Politico, and before that was a freelance writer for publications such as The New York Times, The Washington Post, Smithsonian, Lingua Franca magazine, The New Republic, Slate, and Salon. Earlier in his career, he worked for The Associated Press. Originally published at KFF Health News
For two decades, patients and physicians eagerly awaited a lower-cost version of the world’s bestselling drug, Humira, while its maker, AbbVie, fought off potential competitors by building a wall of more than 250 patents around it.
When the first Humira biosimilar — essentially a generic version — finally hit the market in January, it came with an unpleasant surprise. The biosimilar’s maker, Amgen, launched two versions of the drug, which treats a host of conditions including rheumatoid arthritis. They were identical in every way but this: One was priced at about $1,600 for a two-week supply, 55% off Humira’s list price. But the other was priced at around $3,300, only about 5% off. And OptumRx, one of three powerhouse brokers that determine which drugs Americans get, recommended option No. 2: the more expensive version.
As Murdo Gordon, an Amgen executive vice president, explained in an earnings call, the higher price enabled his company to give bigger rebates, or post-sale discounts, to Optum and other intermediaries. Most of that money would be passed on to insurers, and patients, he said. Gordon did not mention that the higher-priced option would leave some patients paying much more out-of-pocket, undermining the whole rationale for generic drugs.
The Optum-Amgen announcements perfectly elucidated why, after years of thundering against drugmakers, Congress and the administration have now focused on regulating the deal-makers known as pharmacy benefit managers, or PBMs. Sen. Bernie Sanders’ health committee grilled a panel of PBM and pharmaceutical executives Wednesday in preparation for a vote on PBM legislation, expected Thursday.
The three biggest PBMs — OptumRx, CVS Caremark, and Express Scripts — control about 80% of prescription drug sales in America and are the most profitable parts of the health conglomerates in which they’re nestled. CVS Health, the fourth-largest U.S. corporation by revenue on Fortune’s list, owns CVS Caremark and the insurer Aetna; UnitedHealth Group, a close fifth, owns Optum; and Cigna, ranking 12th, owns Express Scripts. While serving as middlemen among drugmakers, insurers, and pharmacies, the three corporations also own the highest-grossing specialty drug and mail-order pharmacies.
“John D. Rockefeller would be happy to be alive today,” said David Balto, a former Federal Trade Commission attorney who represents clients suing PBMs. “He could own a PBM and monopolize economic power in ways he never imagined.”
Drug manufacturers claim that exorbitant PBM demands for rebates force them to set high list prices to earn a profit. Independent pharmacists say PBMs are driving them out of business. Physicians blame them for unpredictable, clinically invalid prescribing decisions. And patients complain that PBMs’ choices drain their pocketbooks.
With PBMs driving prices, competition has had the opposite effect from what economic theory predicted Medicare patients would spend out-of-pocket on drugs, one large study showed. Over a five-year period, patients were paying 50% more for branded drugs that had competitors than for those that didn’t.
All this makes the PBMs ripe targets for politicians of both parties. Yet the complexity and obscurity of their role in the drug marketplace have skeptics wondering whether legislation advancing in the House and Senate will actually help patients or lower prices at the pharmacy counter.
“We may try to make things better and actually make things worse,” Sen. Rand Paul (R-Ky.) said at Wednesday’s hearing.
The PBMs pass along most of their rebates to health plans, which will bear a larger share of patient drug costs in coming years under Medicare changes that are part of the 2022 Inflation Reduction Act. It’s likely that pressure on insurers will be passed along to PBMs and result in even more aggressive limits on physician prescription decisions, said Troyen Brennan, an adjunct Harvard University professor who was chief medical officer for CVS Health from 2008 to 2022.
Several congressional bills target drug company rebates to PBMs and what’s known as “spread pricing” — the extra money PBMs collect from insurers over what they pay pharmacies for drugs.
But those aren’t the big PBM revenue sources anymore, Brennan said. PBMs today mostly make money by owning mail-order and specialty pharmacies and from the government’s 340B program, created to help hospitals that treat a disproportionately elderly and poor population. Medicare requires drugmakers to provide big discounts to participating hospitals and the growing rosters of affiliated physician groups they own, and some of those discounts end up with PBMs.
Employers and the federal government decide where most of the rebate money goes, PBM leaders testified Wednesday — and health plans decide what out-of-pocket costs their covered members will pay.
In other words, drug companies blame PBMs for high drug counter prices, PBMs blame insurers, and insurers blame the drug companies, all part of a health care system that hinges on an unspoken bargain: Make life comfortable for some — mostly the upper and middle classes — at the expense of lower-income and poorly insured people who get what they get.
PBMs’ extraction of money from patients in the name of “copayments” at the pharmacy counter “reintroduces medical underwriting” that was stripped away by the Affordable Care Act, Craig Garthwaite, a health care researcher at Northwestern’s Kellogg School of Management, told a Senate panel last year. Insurers can no longer pick and choose whom to insure, as they could before the landmark 2010 health law. But they are finding ways to make the sickest pay.
“People with expensive conditions are paying more for insurance so healthy people can pay less,” he said.
PBMs Evolve From Minnows to Whales
In 1967, a year before the first PBM was founded, spending on prescription drugs outside of a hospital in the U.S. totaled around $3.3 billion, compared with more than $600 billion in net payments last year. By 2005, when Medicare expanded to include coverage of outpatient drugs, government and private insurers depended on PBMs’ negotiating power to keep rising drug prices in check.
The Federal Trade Commission and Justice Department allowed the largest PBMs to gobble up competitors and merge with insurers during the Bush and Obama administrations on the grounds that bolstering their powers might rein in prices. The FTC fought state investigations of anti-competitive behavior, saying that pressure on PBMs would benefit consumers.
The FTC under President Joe Biden has switched course, at least partly because of the arrival of Chair Lina Khan, a vigorous proponent of antitrust policy who launched an investigation of the PBMs last June.
It came partly at the request of independent pharmacists, who rely on PBM reimbursements for the drugs they purchase and provide consumers. Thousands of pharmacists complained to the FTC that PBMs force them to accept unfairly low reimbursements — then slam them with opaque rules requiring them to pay back some of the money months later. Pharmacists returned $12.6 billion to PBMs in 2021, according to a recent Medicare Payment Advisory Commission report.
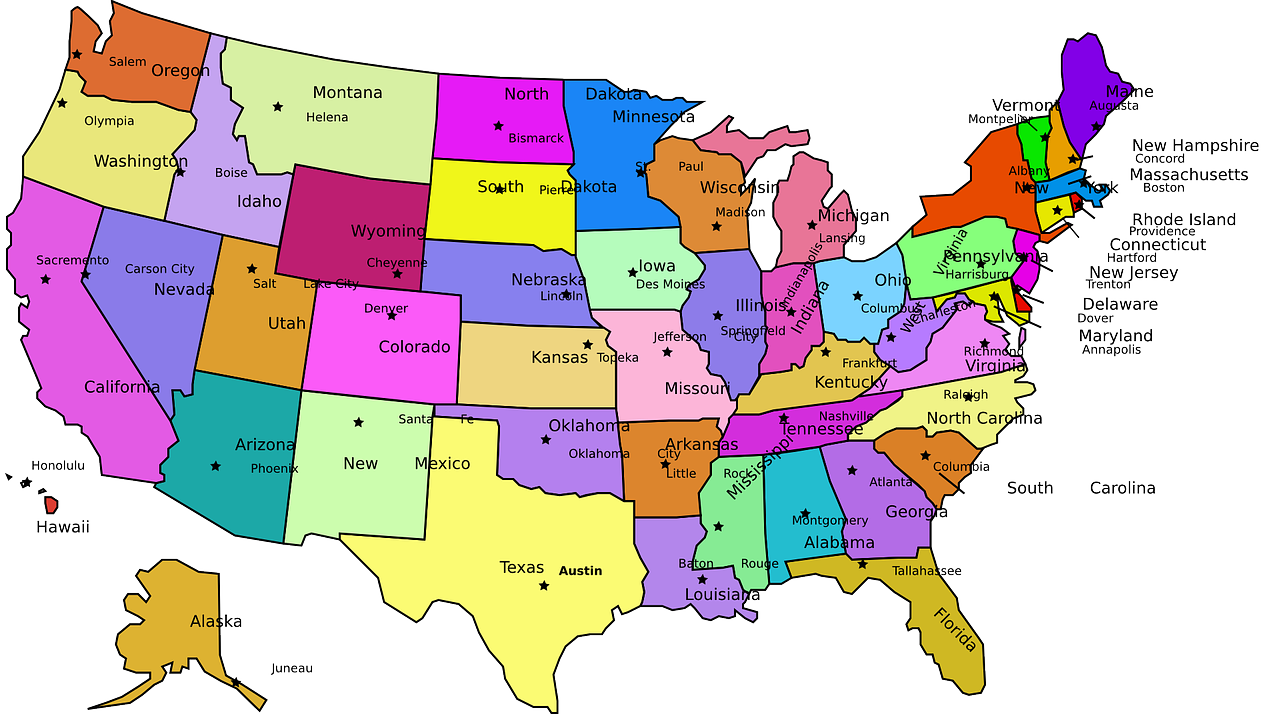
During a recent week, said Ashley Seyfarth, who owns Kare Drug in Aztec, New Mexico, a PBM reclaimed money from one prescription because the paperwork was faxed. It clawed back cash from another sale because Kare had kept the drug on the shelf an extra day, beyond the PBM’s time limit, to accommodate a patient delayed getting to the store.
And her reimbursements are “beyond low,” Seyfarth said. She laughed when asked whether contract terms with the PBMs were negotiable. “You aren’t negotiating anything,” she said. “It’s take it or leave it.”
PBMs “have the right to audit whether contract terms are agreed to,” Angela Banks, vice president of policy at the Pharmaceutical Care Management Association, the PBM trade group, said at a recent conference. “A lot of the complaints about PBMs come from two parties from whom we are extracting money: manufacturers and pharmacists.”
PBM pricing decisions are often murky. According to a recent study, in 2018 Medicare spent $2.6 billion more through PBMs for a year’s worth of 184 generic drugs than they would have cost at Costco. Doctors and hospitals find PBM formularies baffling, with dozens of variations depending on a patient’s health plan.
When Philadelphia-area internist Amy Davis writes a prescription, she has no idea what the pharmacy will bill her patients, she said, or whether a PBM has decided the drug needs prior authorization. Sometimes she doesn’t find out until a patient returns months later saying they skipped the drug because it was too expensive.
“We physicians are completely in the dark,” she said. “And it’s designed that way.”
The PBMs’ growing use of proprietary pharmacies, including mail-order operations, can interfere with the care of patients like Jasmine St. Clair, a 45-year-old restaurant manager and mother of six in Mount Juliet, Tennessee.
In October 2021, St. Clair’s treatment for a rare, non-smoking-related lung cancer was delayed three weeks after PBM giant Express Scripts insisted her prescription be filled by Accredo, the mail-order pharmacy it owns.
In the meantime, her fatigue and lower-back and neck pain became so bad “I couldn’t pick up my daughter, who was 2,” St. Clair said. “And I was really getting scared.”
After St. Clair started the four-pills-twice-a-day regimen, her tumor rapidly shrank. But in January, her husband’s insurance changed and the medications didn’t arrive on time. When she called Accredo to see what was wrong, “they said, ‘You owe $8,000. Would you like to pay by card?’”
The pharmacy attached to her oncology practice straightened out the payment issue and ensured her continued use of the drug, St. Clair said. Her oncologist, Johnetta Blakely, said these are daily occurrences in her practice.
“The problem with the PBMs and the specialty pharmacies they own is that they are so complicated and intertwined it’s hard to figure out what the heck they are doing,” Blakely said. “All this bureaucratic stuff is a distraction and takes away from things I could be doing, like asking Jasmine about her kids.”
What’s the Remedy?
Bipartisan House and Senate bills would require PBMs to reimburse pharmacies serving Medicaid patients based on an authorized price list, rather than using standards that allegedly allow PBMs to lowball pharmacies. The Congressional Budget Office has estimated the bills would save the federal government $1 billion over 10 years. Another Senate bill would require PBMs to report more of their earnings to the FTC, and would ban deceptive and unfair fees.
But PBMs have shown themselves adept at finding ways around regulation. A federal rule scheduled to take effect next year would curtail PBM “clawbacks” on independent pharmacies. But PBM contracts sent out to pharmacies in recent weeks get around that by lowering reimbursement fees and putting a percentage of their payments to pharmacies into a kind of escrow, said Douglas Hoey, CEO of the National Community Pharmacists Association.
When the Trump administration considered banning brand-name drug rebates in 2017, PBMs set up companies in Ireland and Switzerland to take over the negotiations and purchases. Doing so offered a tax advantage and allowed the PBMs to avoid scrutiny of the quantity and nature of those deals. Recently, Express Scripts set up another company to purchase generic drugs, in the Cayman Islands.
And PBMs appear adept at moving money from one pocket to another. “Yesterday’s rebates are today’s fees and potentially tomorrow’s something else,” said John O’Brien, CEO of the pharmaceutical industry-funded research group, the National Pharmaceutical Council.
Every arrangement that PBMs make with manufacturers, employers, and insurers is secret and proprietary, said Barak Richman, a Duke University Law School professor. This makes it nearly impossible to examine what kind of deals PBMs are making.
Antitrust law could be brought to bear on the PBMs, Richman said. And the Biden administration has shown an eagerness to possibly reverse mergers that haveincreased PBM clout. The Justice Department has taken similar steps.
But federal officials will have to move fast to slow the PBMs. Insurers that don’t have PBMs as part of their business have been shrinking in recent years because of the growing clout and buying power of the companies.
“I predict that any health insurer that doesn’t have a PBM is going to disappear in 10 years,” said Neeraj Sood, a professor at the University of Southern California Sol Price School of Public Policy. “Otherwise, there is no way to compete with the big three.”
______
1 I really now hate the way Medicare inserts itself into my payment relationship with my doctor. That gives Medicare the right to see my doctors’ records on an ongoing basis, while with my old plan, they could not demand records but my doctor could elect to send more information if my insurer was giving me a hard time about paying a claim.