Yves here. KLG focuses today on an important topic: the world rise in cancers among younger people. Note that the key papers he discusses, one published in 2022, the other 2024, both built data sets for time periods Before Covid (for the 2024 paper, from 2010 to 2019). That means the trends have gotten even worse since then. IM Doc has seen in his own practice a marked rise in cancers, particularly ones once considered exotic, as well as particularly fast-moving ones in the After Covid era. His observations are confirmed by oncologists in tertiary medical centers.
Although no one seems to know the causes of this shift, Anthony Leonardi has offered a plausible thesis, that of T-cell depletion. In simple layperson terms, T-cells are a second line of defense against pathogens. T-cells also police the body for cancers and stop the cancers we are growing all the time from becoming dangerous. T-cells do not replenish in adults.
Leonardi has argued that Covid taxes and may even deplete T-cells. More cases of Covid lead to weakened immune defenses, including against the recurrence of Covid as well as other infectious diseases. And that would also produce a greater risk of cancer.
Note that it is possible, but again not proven, that the Covid vaccines could also produce this effect. Recall that the mRNA vaccines produced such a strong immune system response that even healthy young people often had to take a day or two off from work.
So we have a serious rise in an underlying pathology apparently kicked into higher gear by Covid. And the more recent increase, if acknowledged, may take the focus of the underlying trend, which KLG points out could be addressed….if officials took serious interest in the lifestyle issues that promote obesity.
KLG’s introduction:
Younger and younger people are getting cancers that have been previously more prevalent in an older cohort. The most likely reason is that younger people are exposed to risk factors that were not there for their parents and grandparents. One primary risk factor is epidemic obesity, which puts the body in a chronic inflammatory state that is conducive to cancer progression. More than 20% of Americans are now living with obesity. This presents health problems, but epidemic obesity is also a problem of the political economy of diet and lifeways, Therefore, while directed medical approaches are essential, reduction of the burden of early-onset cancer is also a problem of political economy. This makes the problem more difficult but also more tractable. As the US government turns over in the next several weeks, it will be essential to pay attention and hold Make America Healthy Again accountable.
By KLG, who has held research and academic positions in three US medical schools since 1995 and is currently Professor of Biochemistry and Associate Dean. He has performed and directed research on protein structure, function, and evolution; cell adhesion and motility; the mechanism of viral fusion proteins; and assembly of the vertebrate heart. He has served on national review panels of both public and private funding agencies, and his research and that of his students has been funded by the American Heart Association, American Cancer Society, and National Institutes of Health
A search using “cancer in young people” as the query returns a long list of hits. Articles in the popular press are often over the top, but epidemic or not, this is a real concern. The primary question is “What to Know About Rising Rates of ‘Early-Onset’ Cancer.” The scientific literature on this topic is large, and two recent comprehensive articles, both available to all readers, cover the subject well.
Before getting into the evidence, a few reminders about the origins and nature of cancer may be useful: Cancer is a multistep process that begins with a mutation leading to dysregulated proliferation [1] of the mutant cell. This initial mutation is followed by others that further enhance proliferation and cancer progression. Subsequent mutations may also allow cancer cells to move to other places in the body and seed new tumors. For example, liver metastases from the primary colon tumor are often the cause of death in these patients. My father died of a brainstem tumor that was secondary to his lung cancer, which was acquired by the usual exposure to mutagens. Cancer therapies [2] have been developed to interfere with every stage of cancer progression, and the successes of clinical oncology for many cancers have been spectacular since the National Cancer Act was signed by Richard Nixon fifty-three years ago. Nevertheless, cancer remains the second-leading cause of death in the USA, and most cancers are caused by an environmental insult of some kind.
The first article is a comprehensive retrospective and prospective review: Is early-onset cancer an emerging global epidemic? Current evidence and future implications (Ugai et al. 2022). It was published in October 2022 in Nature Reviews: Clinical Oncology by an international team of authors. Key Points of this paper include:
- The incidence of cancers of various organs diagnosed in adults ≤50 years of age has been rising in many parts of the world since the 1990s.
- Evidence suggests an etiological role for risk factor exposures in early life and young adulthood, although specific effects of individual exposures remain largely unknown.
- The early life exposome (including, among other factors, diet, lifestyle, obesity, environmental exposures and the microbiome) has changed substantially, with variable trends observed around the world since the mid-20th century.
- The early-onset cancer epidemic might be one manifestation of increasing trends in the development of many chronic diseases in young and future generations.
- Raising awareness of the early-onset cancer epidemic and improving the early-life environment should be our immediate goals: these are likely to reduce the burden of both early-onset and later-onset cancers.
Although cancer screening has improved, this implies that novel environmental risk factors in early life (from conception) and childhood lead to early-onset cancers, as shown in Figure 2.
Most of these risk factors are well known. Their relationships, some of which are not completely understood yet, to early-onset cancers are described in this lightly edited excerpt from Table 1.
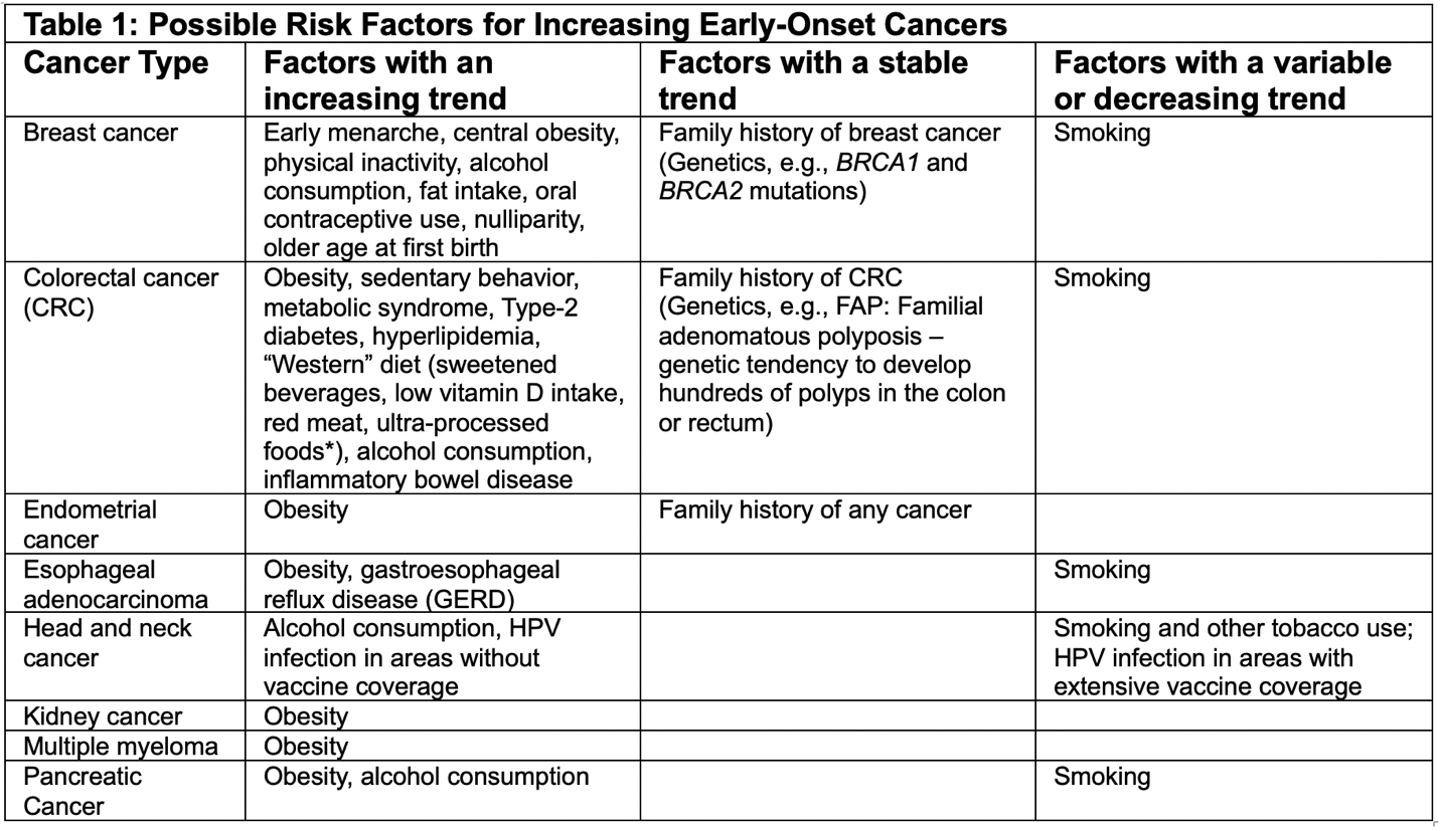
The key to this perspective is that the relevant risk factors with an increasing trend are often behavioral, whether intentional or not.
For example, early-onset colorectal cancer (CRC) has been linked to high adulthood BMI. [3] Studies have also shown that high childhood or adolescent BMI predisposes one to early-onset CRC. Sedentary lifestyle and physical inactivity are correlated with early-onset CRC. Since obesity and a sedentary lifestyle with little physical inactivity are commonly linked, this makes perfect sense. As noted in Table 1, obesity is a risk factor for endometrial cancer, esophageal cancer, kidney cancer, multiple myeloma (a form of leukemia), and pancreatic cancer. Obesity causes a generalized chronic inflammatory condition that leads to responses characterized by cell proliferation and other abnormal states For example, cell/tissue changes in the esophagus caused by gastroesophageal reflux disease (GERD/heartburn) can progress directly to esophageal cancer (average 5-year survival rate: 20%), which is why symptomatic relief of heartburn is not sufficient to prevent progression of GERD to cancer.
Current evidence on early-onset breast cancer shows “the trend of reproductive factors, central obesity, physical inactivity, alcohol consumption and dietary westernization since the mid-20th century might have contributed to the rising incidence of premenopausal breast cancer.” For example, earlier menarche may be due to the Western diet. The molecular signatures of pre- and postmenopausal breast cancers are also different, which is further evidence that early-onset breast cancer is a distinct disease.
All of this goes together with changes in the “Western” diet, especially in the United States over the past 50-60 years. Thus, it is unsurprising that the increase in early-onset CRC has accompanied the obesity epidemic during this period. As covered before in this series [4], when dietary fat (lipids) and cholesterol (which is not a fat but the two are usually conflated) were demonized in response to the Diet-Heart Hypothesis, fat calories were replaced by carbohydrates. This is undoubtedly the proximal cause of the obesity epidemic, which may also have been aggravated by the prevalence of ultra-processed foods (UPF) in the Western diet. [5]
Ugai et al (2022) are very convincing in their description of the epidemic in early-onset cancer in young people below the age of 50. But what do the population data say? This has been addressed in Differences in cancer rates among adults born between 1920 and 1990 in the USA: an analysis of population-based cancer registry data (Sung et al. 2024) published in Lancet Public Health in August 2024. They begin with the following Summary:
- Trends in cancer incidence in recent birth cohorts largely reflect changes in exposures during early life and foreshadow the future disease burden…we examined cancer incidence and mortality trends, by birth cohort, for 34 types of cancer in the USA.
- Data were extracted for 23,654,000 patients diagnosed with these 34 types of cancer and 7,348,137 deaths from 25 of these cancers for individuals.
- 17 of the 34 cancers had and increasing incidence in younger birth cohorts, including nine that previously had declining incidence in older birth cohorts. These findings add to the growing evidence of increased cancer risk in younger generations, highlighting the need to identify and tackle underlying risk factors.
These data are congruent with previous research: “Ten of 17 cancers with increasing incidence in younger birth cohorts are obesity-related cancers (colorectum, kidney, gallbladder and other biliary, uterus, pancreas, gastric, estrogen-positive breast, ovary, myeloma, and liver), suggesting a potential role of obesity (and the obesity epidemic) in emerging cancer trends in recent generations.” (lightly edited) The data presented in the paper are very clear but difficult to transfer.
In addition to their agreement with the obesity hypothesis, Sung et al. also discuss the linkage between the gut microbiome and gastrointestinal cancer and how the Western diet and overuse of antibiotics have altered the gut microbiome in the younger birth cohorts. The microbiome and early-onset cancer are covered in a recent open-access paper: The microbiome and rise of early-onset cancers: knowledge gaps and research opportunities (2023). Microbial dysbiosis caused by environmental insult leads to heightened oxidative stress and inflammation.
Hopeful notes in their data include the accelerated downturn in cervical cancer due to the effectiveness of vaccination against HPV. Women born in 1990 were ~16 years old when HPV vaccination was approved for women and girls aged 9-26 years in 2006. Wider adoption of HPV vaccination should reduce the incidence of HPV-caused cancers in both sexes. Tobacco-associated cancers are also down in the younger birth cohorts due to the rapid decline of smoking in these groups, although the deleterious health effects of smokeless tobacco (cancer) and vaping remain.
Taken together, the results described here show that during the second half of the twentieth century successive birth cohorts have shown increased incidence of common cancer types that have different origins. The findings of both papers highlight the significance of early exposure to risk factors in this cancer burden. More importantly, the data also indicate that avoidance of environmental insults and changes in behavioral risk factors will prevent much of the early-onset cancer in future birth cohorts.
So, what are we to do about early-onset cancers? A general scheme is illustrated in Ugai et al., Figure 3. As an outline, this is very good. As a political plan, not so much. But that is not up to the authors. Rather, it is up to all of us.
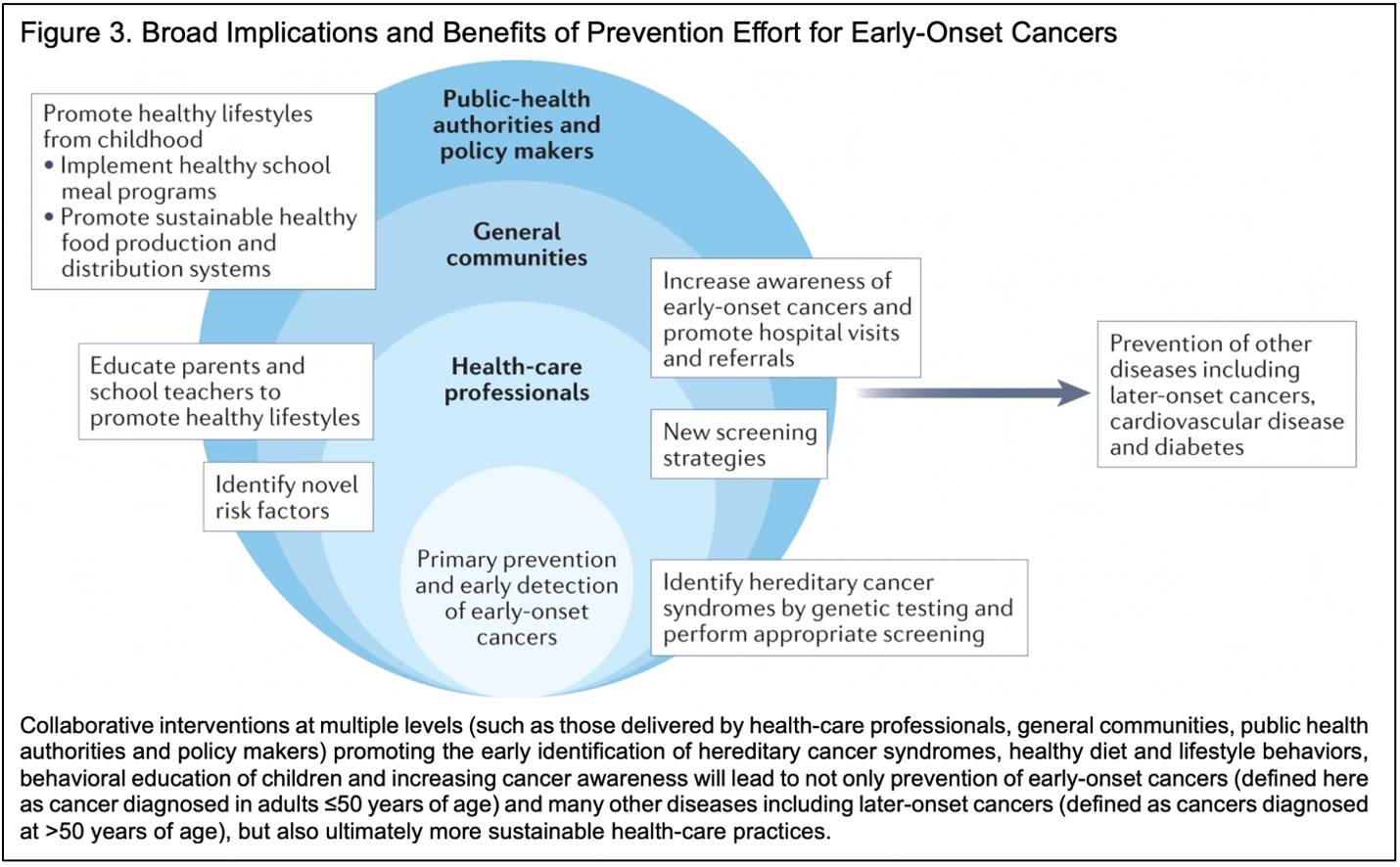
Starting from the upper left box and leaving the other conventional recommendations for another time, how will it be possible to promote healthy lifestyles from childhood? Bullet point the first: Implement healthy school meal programs. Yes, this is very desirable. But it is not possible now in the United States. When I was an elementary school student, the “lunchroom ladies,” who were loved by students and teachers alike, actually cooked lunch every day. Three out of five days the entire building was suffused with the aroma of yeast rolls made from scratch. On hot dog day, the slaw and cinnamon buns were made from scratch. Same for what they called pizza (it wasn’t recognizable as such, but it was good). Raw celery, carrots, apples, oranges, plums, grapes, and bananas were common. Students drank water or milk. An extra glass of milk was five cents. This continued into junior high school (middle school). Selections were more varied in my public high school, and many went to the new McDonalds for lunch. But the kitchen still functioned as a kitchen instead of an oven attached to a large walk-in freezer that had been stocked with ready-to-thaw ultra-processed food-like substances.
Things have changed over the past 30+ years. This is not the place for an extended discussion but these fifteen lunches from around the world illustrate the issue. Thirteen, possibly fourteen, of the countries have a serious food culture and expect everyone to partake, especially the children if these meals really are illustrative (admittedly a legitimate question). One country, #15, does not. But, somewhat breathlessly, in the US “Multiple lunch options like salads, sandwiches, soups, smoothies, pasta, pizza + so much more. With over 20+ choices a week, the combinations are endless, making lunch anything but typical!”
We could do with more typical if typical were like the other school lunches. Other search results are similar. In this array, with some duplicates from the first, Country #1 this time is serving green peas from a can, fruit in syrup, and breaded mystery nuggets with ketchup. So, will Big Ag and Big Food and the Big Distributors “allow” US schools to approximate what may be the practice in France, Brazil, Greece, Spain, India, or Italy from the first array? That is the question. The command to “Move fast and break things” is called for once again, but masters of things that must be broken are unlikely to acquiesce.
Bullet point the second: Promote sustainable healthy food production and distribution systems. Another laudable goal, but one that industrial agriculture cannot meet, by definition, and most certainly would not if it could. Industrial agriculture is a category mistake that has nothing to do with healthy food and everything to do with wealth extraction.
Thus, early-onset cancer is a problem of political economy as much, or more, as it is a problem of medicine and health. This leads us to our current politics, in which Make America Healthy Again (MAHA) and its people have big plans. MAHA is constituted as a PAC – Political Action Committee – apparently with two current websites, here and here. Senator Roger Marshall, MD (R – Kansas) recently formed the Congressional MAHA Caucus:
Today (19 Dec 2024), U.S. Senator Roger Marshall, MD, a member of the Senate Health, Education, Labor, and Pensions (HELP) Committee, announced the creation of the Congressional Make America Healthy Again (MAHA) Caucus. This new caucus will focus on nutrition, access to affordable, high-quality-nutrient-dense foods, improving primary care, and addressing the root causes of chronic diseases. (emphasis added)
As in the entire healthcare discussion, “access” does a lot of work here, but the focus on nutrition, primary medical care, and the root causes of chronic disease is absolutely correct. The details matter, however, and one of the major MAHA influencers seems to be Casey Means, MD, [6] who published Good Energy: The Surprising Connection Between Metabolism and Limitless Health along with her brother in May 2024 (NB: I have not read this book, which is on order; therefore much of what follows is from the Amazon link). Good Energy represents:
A bold new vision for optimizing our health now and in the future. (emphasis in original)
What if depression, anxiety, infertility, insomnia, heart disease, erectile dysfunction, type 2 diabetes, Alzheimer’s, dementia, cancer and many other health conditions that torture and shorten our lives actually have the same root cause? Our ability to prevent and reverse these conditions – and feel incredible today – is under our control and simpler than we think. The key is our metabolic function – the most important and least understood factor in our overall health. As Dr. Casey Means explains in this groundbreaking book, nearly every health problem we face can be explained by how well the cells in our body create and use energy. To live free from frustrating symptoms and life-threatening disease, we need our cells to be optimally powered so that they can create “good energy,” the essential fuel that impacts every aspect of our physical and mental wellbeing. (emphasis added)
It would be silly to say that good nutrition is irrelevant to how the body handles any condition or that poor nutrition can lead to disease, with heart disease and Type-2 diabetes as prime examples. But to say that that cancer and Alzheimer’s disease have the same root cause, and that this is due a lack of “good energy” is ridiculous. Metabolic energy is energy. Not having enough is indeed a problem, but I will have to read the book to learn the meaning of “bad energy,” forthcoming. MAHA world is likely to be a place of never-ending wonder.
Still – to eat well, get enough sleep, have a rewarding job with the expectation of a comfortable retirement, to know that your children are not severely at risk in the coming world, and to not have an overwhelming dread that one illness can bankrupt you if your “access” to health care is denied – is to live a good life. These are problems of political economy. They are currently unsolvable under the Neoliberal Dispensation in which “the market” is the measure of all things, even those that cannot be measured. What politicians of the Uniparty fail to realize is that virtually all of us already have “skin in the game.” But maybe MAHA-PAC can be as successful the many other PACs operational today. Several come readily to mind.
Finally, as an aside, the blurbists for Good Energy are the usual suspects, although Robert H. Lustig was a minor surprise. One who is not well known but should be is Will Harris of White Oak Pastures in Bluffton, Georgia (pop. ~115). He is a visionary farmer and businessman with the deepest roots in his community:
“In Good Energy, Dr. Means makes a bold case for why food – and particularly regenerative agriculture – must be at the very center of healthcare. She has emerged as one of the strongest physician voices teaching doctors and patients that we will never achieve optimal human health without optimal soil health and biodiversity – a message that the healthcare system would be wise to pay attention to. Dr. Means makes it clear that we can’t drug our way out of a broken food system.”
This is exactly right, and the case has been made by Wendell Berry and Wes Jackson since the 1960s, and F.H. King(Farmers of Forty Centuries, pdf) and Liberty Hyde Baily (The Holy Earth) long before. But it also illustrates the problems we face. White Oak Pastures is the wave of the future, if only a ripple now, especially as the world gets smaller in the coming inconvenient apocalypse. But it cannot serve the local or regional community and compete with an industrial livestock industry (sic) in which >90% of yearling cattle, according to a friend who works for the Georgia Department of Agriculture, in Georgia are shipped to feedlots in the Great Plains to be finished with industrial commodity grain, followed by the product being shipped back from where it came. [7]
Under the Neoliberal Dispensation, the negative externalities associated with industrial agriculture are left unaccounted for in retail prices, by design. The only White Oak Pastures product available locally at retail is their grass-fed lean ground beef. It is very good and I use it often even though yesterday the price was $11.49 per pound, about 30% more than industrial ground beef and up from $8.99 (28%) during the Biden Inflation. I recognize the ability to keep my money in the regional economy is conditional on being a member of the Professional Managerial Class – PMC. However, if there were 20-100 White Oak Pastures in each of these United States, the possibilities for our entire political economy would have few limits. And be much better for the health of the people and planet Earth, the sooner the better.
What remains to be seen as the US government turns over in the coming weeks is whether MAHA-PAC can have a larger reach than the more likely MAHA-PMC-PAC. If MAHA-PAC succeeds, early-onset cancer and a large host of other sociogenic health problems can be solved.
It’s up to the citizenry to make this happen. Somehow.
Notes
[1] Cancers are often said to consist of “rapidly growing cells.” While the length of the cell cycle of a cancer cell may be slightly shorter than that of the normal cell, both cells take about 24 hours to divide after the process begins. The problem with cancer cells is they continue to divide when they are not supposed to, not that they divide/grow faster.
[2] Their development is covered by Siddhartha Mukherjee very well in The Emperor of All Maladies. His books on the cell and the gene are also excellent contemporary treatments for the general reader.
[3] Body mass index (BMI) is an imperfect measure of obesity. Many with a high BMI are very physically fit, such as the power lifter I knew with a BMI in the “obese” range. He could deadlift more than 500 pounds and run as many 6-minute miles as he wanted. But BMI is useful as a general measure of the spectrum from “low-weight to over-weight to obese.”
[4] Including: The Diet-Heart Hypothesis and Carbohydrates, The Diet-Heart Hypothesis and Cholesterol, Industrialism is Bad for Our Health.
[5] Note that UPF was added Table 1, as indicated by the asterisk. UPF are included in the paper but attention to UPF has increased markedly since this paper was published. The book on UPF has been discussed in Ultra-processed People in an Ultra-Processed World.
[6] From Amazon: “Casey Means is the Chief Medical Officer and co-founder of Levels, a health technology company with the mission of reversing the world’s metabolic health crisis. She has been on faculty at Stanford University, lecturing on metabolic health and health technology. She received her undergraduate degree with honors from Stanford, where she was President of her class. She graduated from Stanford Medical School and trained in Head & Neck Surgery at Oregon Health and Science University before leaving traditional medicine to devote her life to tackling the root cause of why Americans are sick.” As noted in her Wikipedia entry, “Means withdrew from her medical residency at age 30. She has attributed this decision to the lack of training she received about nutrition and the underlying causes of chronic disease. Means dedicated her practice to functional medicine, a marketing term associated with medical practices that are not science-based.” That she did not complete her residency means that Dr. Means cannot properly identify herself as a physician. From STAT the relevant passage reads: “Casey dropped out of medical residency on her 30th birthday. It’s a cinematic story, retold often: She was in the operating room, gazing down upon a child with incessant sinus inflammation, and disturbed that she didn’t know what was causing it – something she says she never learned. Means realized she was never taught about nutrition as a therapeutic tool, either. (This last assertion is disputed by a fellow Stanford-trained doctor, neurosurgeon Tyler Cole, who graduated around the same time as Means.) Casey became a functional medicine doctor, focused on holistic approaches to care, and editor of the International Journal of Disease Reversal and Prevention. She later started Levels.
[7] It would seem that a large part of the carbon footprint of cattle “farming” lies in this madness.


